A note of acknowledgement
We would like to thank the patients and families whose experiences are documented in this report. We would also like to thank the healthcare staff and external organisations who engaged with the investigation for their openness and willingness to support improvements in this area of care.
About this report
This report is intended for healthcare organisations, healthcare staff, policymakers, higher education institutions and the public to help improve patient safety in how 12-lead electrocardiograms (ECGs) are carried out in ambulance services.
The investigation considered the use of ECGs to help identify ST elevation myocardial infarction (a type of heart attack) and the support available to ambulance crews in making this identification. The findings may be applicable to other areas of practice when considering how clinical decision making is supported.
Executive summary
Background
This is the second of two investigation reports exploring the use of 12-lead electrocardiograms (ECGs) in ambulance services. An ECG is a test that records the electrical activity of a patient’s heart, it needs to be correctly carried out and accurately interpreted by clinicians to determine the patient’s condition and potential diagnosis.
This investigation looked at how patients with suspected ST elevation myocardial infarction (STEMI) (a type of heart attack) are diagnosed. It explored the clinical advice and support available to ambulance crews, including the design, functionality and use of 12-lead ECG equipment to aid clinical decision making. This included looking at monitor/defibrillator devices (which monitor a patient’s heart activity and can be used to deliver a shock to restore their heart rhythm if needed) and auto-interpretation (software that analyses a patient’s ECG waveform to help clinicians interpret ECG readings).
The first investigation report was published in March 2025 and looked at paramedic education, training and competence in ECG practice, and the task of carrying out and interpreting a 12-lead ECG in the context of the patient’s clinical signs and symptoms.
The investigation
HSSIB received a prevention of future deaths (PFD) report, issued by HM Coroner in November 2023, which raised concerns about the ability of ambulance crews to correctly interpret a 12-lead ECG and how auto-interpretation software on monitor/defibrillators was used to help inform clinical decision making. HSSIB did not investigate the incident reported in the PFD. Instead, the investigation considered the PFD along with multiple other sources of evidence to help identify potential patient safety risks.
The investigation spoke to key stakeholders to understand the safety risks associated with interpreting ECGs, specifically in relation to STEMIs. The way 12-lead ECGs are undertaken and interpreted was identified as a growing area of concern, with safety risks that can have a significant impact on outcomes for patients. These risks included environmental factors that affected the accuracy of ECG readings, ambulance crews’ levels of experience and the availability of advice to help them make a diagnosis, and interpretation and application of guidance around heart attacks.
Findings
Monitor/defibrillator equipment and auto-interpretation
- Monitor/defibrillator auto-interpretation algorithms were not designed to replace clinical decision making by a suitably experienced clinician, but ambulance crews may choose to use them to help diagnose patients with a potential STEMI.
- The accuracy of monitor/defibrillator algorithms, when diagnosing STEMI, dropped significantly for borderline cases which is when ambulance crews needed the most assistance.
- There was variability in the ECG printouts produced by monitor/defibrillator devices, with some described as being easier to interpret than others.
- Environmental influences such as other nearby electrical devices, or patient movement, affected the readability and perceived reliability of the ECG trace for STEMI diagnosis, and the accuracy of the auto-interpretation.
- Placement of electrodes on patients’ bodies was inconsistent, which could alter the shape of the ECG waves and affected the ability of ambulance crews and the auto-interpretation to diagnose a STEMI correctly.
- Monitor/defibrillators have evolved over time and their main function is now for monitoring rather than as defibrillators.
- Procurement processes have limited focus on the monitoring and cardiac diagnostic functions of monitor/defibrillator devices, such as ease of use, how information is displayed and the reliability of the auto-interpretation in helping ambulance crews diagnose STEMI.
- Information about the age and sex of a patient was not always entered into the monitor/defibrillator which can then lead to the auto-interpretation statement providing an incorrect analysis for that patient.
- ECG interpretation algorithms did not account for differences in ethnicity due to a lack of research globally.
Clinical advice and support in ambulance trusts
- The set-up of clinical support hubs for ambulance crews varied between ambulance trusts. These hubs had begun to evolve from a service initially designed to support newly qualified paramedics, into a service offering a second opinion to all ambulance crews on a diagnosis, including advice about ECG interpretation and suspected STEMI.
- Paramedics on ambulance service clinical advice lines providing advice on suspected STEMI typically had no additional specialist education, training, or experience in ECG interpretation.
- Paramedics in the clinical support hub were able to access most ECG traces, but did not have access to patients’ medical histories or the holistic view of a patient available to ambulance crews at the scene.
Clinical advice and support from primary percutaneous coronary intervention (PPCI) centres
- PPCI centres had limited capacity to provide ECG interpretation advice to ambulance crews as they were not commissioned to provide this service.
- PPCI centres interpreted acceptance criteria differently, causing confusion for ambulance crews about whether the centres would accept patients or not, particularly in the case of evolving STEMIs.
- PPCI centres that had implemented two-way communication, to allow for the provision of specialist cardiology advice about suspected STEMI to ambulance crews, had reduced the number of false activations of PPCI teams, which enhanced patient care and increased the centres’ efficiency, reducing costs and fatigue in those teams.
HSSIB makes the following safety recommendations
Safety recommendation R/2025/071:
HSSIB recommends that NHS Supply Chain reviews and amends the procurement framework for monitors/defibrillators to help ambulance services ensure they are fully considering the defibrillation/monitoring and cardiac diagnostic functions of the device when making purchasing decisions, to better reflect how these devices are used in practice.
Safety recommendation R/2025/072:
HSSIB recommends that NHS England/Department of Health and Social Care reviews and amends the service specification for primary percutaneous coronary intervention (PPCI) centres, to include a requirement for a function enabling two-way communication with ambulance crews for shared decision making about patients with a suspected STEMI. This is to ensure that patients are taken to the correct place of care and PPCI teams are responding to confirmed STEMI cases.
HSSIB makes the following safety observations
Safety observation O/2025/075:
Regulatory bodies can improve patient safety by supporting standardisation across manufacturers in how information from ECG traces is displayed.
Safety observation O/2025/076:
Manufacturers can improve patient safety by identifying the potential design barriers and enablers for ambulance crews entering information about a patient’s age or sex into a monitor/defibrillator. This could inform future device design to increase the likelihood that this information is entered when carrying out a 12-lead ECG using auto-interpretation.
Safety observation O/2025/077:
Algorithm developers can improve patient safety by collecting data from different ethnic groups across different geographical locations to help increase the global representation and accuracy of auto-interpretation algorithms for STEMI.
Safety observation O/2025/078:
Ambulance services can improve patient safety by informing regulators and manufacturers of instances where the use of monitor/defibrillators has impacted on patient safety.
1. Background and context
1.1 Introduction
1.1.1 This investigation focuses on how patients with suspected ST elevation myocardial infarction (STEMI) (a type of heart attack) are diagnosed. A STEMI is where a complete blockage of an artery results in the blood supply to a person’s heart being interrupted. This requires emergency treatment at a primary percutaneous coronary intervention (PPCI) centre, where the coronary artery is unblocked to restore blood flow and minimise damage to the heart muscle.
1.1.2 Stakeholders told the investigation that it was often easy to interpret obvious or “barn door” STEMIs from a 12-lead ECG. However, it was more challenging to identify STEMI in patients with less obvious signs and symptoms. The investigation focused on understanding the support available to help ambulance crews’ clinical decision making about potential STEMI. Details of the investigation approach are set out in the appendix.
1.1.3 As part of its terms of reference the investigation explored:
- the design, functionality, and use of auto-diagnostic software to aid clinical decision making
- the clinical advice and support available to ambulance crews in interpreting ECGs for suspected STEMI
- the approach taken in clinical advice, support, and auto-diagnostic software in the consideration of ECG interpretation across protected characteristics (such as age, sex and disability).
1.1.4 The report of the first part of this investigation, ‘12-lead electrocardiograms (ECGs) in ambulance services: paramedic education, training and competence’, was published in March 2025 (Health Services Safety Investigations Body, 2025).
1.2 Background to the investigation
1.2.1 HSSIB received a prevention of future deaths (PFD) report, issued by HM Coroner in November 2023, about an incident involving a woman aged 29 years with chest pain who later died of a heart attack. PFD reports can be issued to interested parties (including a person, organisation, local authority, government department or agency) where HM Coroner believes that action should be taken to prevent future deaths (Courts and Tribunals Judiciary, n.d.).
1.2.2 The PFD report highlighted concerns about the ability of paramedics to interpret a 12-lead ECG and how auto-interpretation software on monitor/defibrillators (see 1.5.2) was used to help inform clinical decision making. HSSIB did not investigate the incident reported in the PFD. Instead, the investigation considered the PFD along with multiple other sources of evidence to help identify potential patient safety risks.
1.2.3 The way in which ambulance crews undertake and interpret 12-lead ECGs was identified by stakeholders as a growing area of concern, with systemic safety risks that can have a significant impact on the outcome for patients. Reliance is placed on these crews to be able to accurately perform and interpret 12-lead ECGs (see 1.4) to support their clinical decision making, taking into account the patient’s overall clinical condition and past medical history.
1.3 ST elevation myocardial infarction
1.3.1 As described in 1.1.1, a STEMI is a type of heart attack. This requires emergency treatment at a primary percutaneous coronary intervention (PPCI) centre, where the coronary artery is unblocked to restore blood flow and minimise damage to the heart muscle.
1.3.2 PPCI is the primary definitive treatment option in England for a STEMI. It involves an initial procedure, known as a coronary angioplasty, to widen the blocked coronary artery. This is done by inserting a tube (catheter) with a balloon at the end through a larger artery in a person’s groin or arm. Once in position at the site of the blocked artery, the balloon is inflated to widen the artery and allow the insertion of a stent (a wire mesh tube).
Figure 1 Normal versus STEMI heartbeat pattern on an electrocardiograph reading
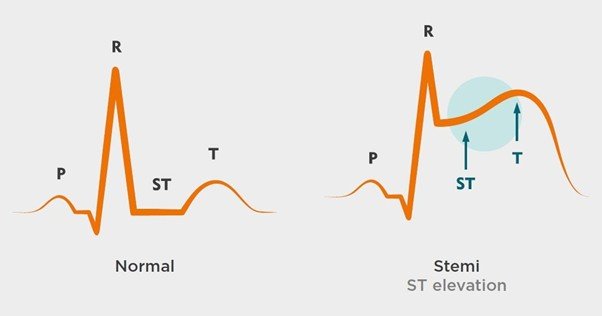
1.3.3 Identifying and treating STEMI is a time-critical task. Guidance from the National Institute of Health and Care Excellence (2020) advises that the preferred treatment option for a confirmed STEMI is PPCI where:
- the patient is seen by medical professionals within 12 hours of the onset of their symptoms, and
- PPCI can be delivered within 120 minutes of the time when thrombolysis (an alternative but less effective treatment used to dissolve blood clots) could have been given to the patient.
1.4 How an ECG is carried out
1.4.1 An ECG is a test that measures and records the electrical activity of a person’s heart, including the rate and rhythm. It is one of the most common heart tests and is the only way for paramedics to identify certain problems with the heart’s electrical impulses.
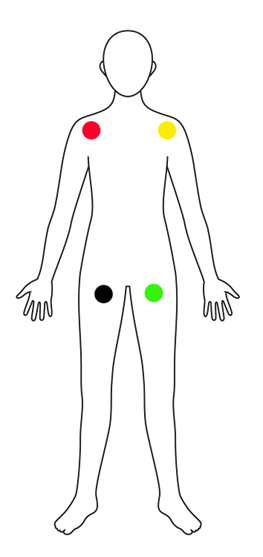
1.4.2 A 12-lead ECG usually involves the placement of 10 electrodes on a patient’s body to record 12 different views of their heart’s electrical activity. This involves accurately placing leads on a patient’s torso and on their arms and legs (see figures 2, 3 and 4). ECGs can also be carried out with fewer electrodes for monitoring purposes, but these provide a more limited view of the heart’s activity and are not considered in this report.
Figure 2 Placement of electrodes on a patient’s torso to record a 12-lead ECG
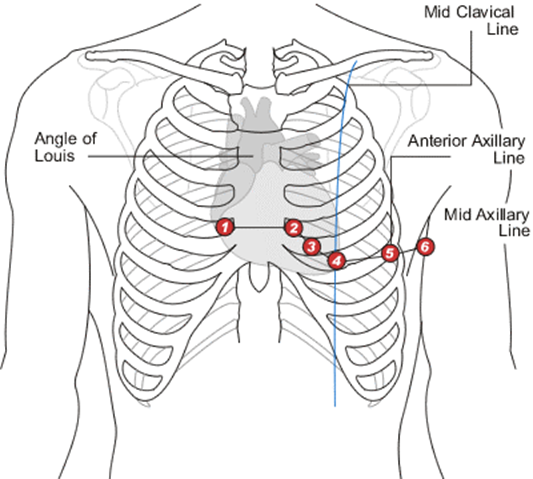
Figure 3 Placement of electrodes on a patient’s arms and legs to record a 12-lead ECG

Figure 4 Alternative electrode positions if limb placement is not available or for ECG monitoring purposes only
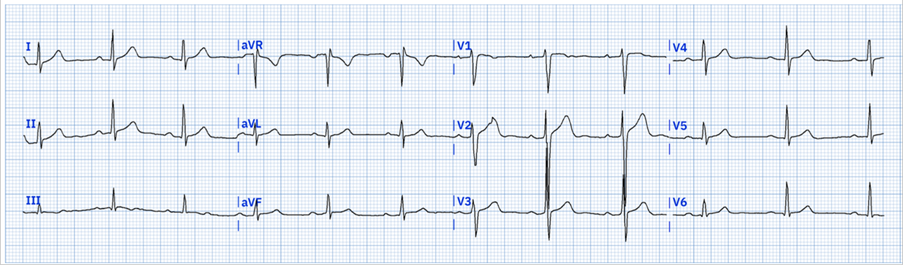
1.4.3 Once electrodes are applied, a 12-lead ECG provides results to clinicians, in the form of a graph known as a ‘trace’ which is displayed on a screen and should be printed out for interpretation. Accurate interpretation is required to determine what activity is being recorded in different parts of the heart (see figure 5).
Figure 5 Example of a 12-lead pre-hospital ECG reading
1.5 Monitor/defibrillator equipment and auto-interpretation
1.5.1 A range of manufacturers provide monitor/defibrillators to the NHS, each with different physical designs, software, functionality and usability. The monitor/defibrillators considered during this investigation were portable and were primarily designed for use by ambulance crews. They can be used to carry out ECGs, including 12-lead ECGs to help diagnose heart abnormalities such as STEMI.
1.5.2 Some monitor/defibrillators provide an auto-interpretation function (also known as auto-diagnostics) to help clinicians interpret an ECG trace. Typically this process has involved the use of software that can identify heart rhythms and patterns, combined with stored data that the device can refer to, to help identify normal and abnormal ECGs. Once identified, the software alerts the user to any potentially abnormal ECG readings or may report a normal ECG.
2. Patient safety incidents and harm
2.1 The following patient stories are shared to identify where organisations have reported concerns about how ST elevation myocardial infarction (STEMI) is diagnosed. This includes where concerns have been raised about how the auto-interpretation function of monitor/defibrillators has been used to inform clinical decision making.
2.2 These vignettes were also used in the first investigation report to highlight concerns about paramedic education, training, and competence in undertaking 12-lead electrocardiograms (ECGs).
Patient 1 (as described in HM Coroner prevention of future deaths (PFD) report)
2.3 An ambulance crew was called out to a woman, aged 29 years, who was vomiting and experiencing chest and arm pain. On arrival the crew noted the patient’s vital signs, which included her blood pressure, pulse and respiratory rate, as ‘normal’. A 12-lead ECG was carried out and the machine’s auto-diagnostic function indicated that the ECG was abnormal and that the patient was likely having an anterior infarct (a heart attack caused by blockage of one of the arteries that supplies blood to the heart).
2.4 The paramedic and emergency medical technician (EMT), both of whom had over 8 years’ experience, interpreted the ECG as ‘normal’ and reported this to the patient. Based on that information, the patient decided not to go to hospital. Later the same day, a second ambulance crew was called out to the patient; they found her in cardiac arrest and were not able to save her life.
2.5 The trust’s incident report noted the ambulance crew had felt reassured about the patient’s condition. This was due to the ‘patient’s age’ and because she ‘appeared well’. The ambulance crew were also reported to have considered that some of the patient’s symptoms were related to another ‘ongoing medical issue’.
2.6 The PFD highlighted the interpretation of a 12-lead ECG and the use of the auto-diagnostic function as matters of concern. HM Coroner noted that interpretation of a 12-lead ECG was a ‘fundamental part of the job of a paramedic’, and highlighted concerns in what the auto-diagnostic report showed in relation to the treatment plan that was followed.
Patient 2
2.7 An ambulance crew, comprising a paramedic and EMT, was called out to a woman aged 85 years. On arrival the crew documented that she ‘had been experiencing nausea for a duration of 2 hours, accompanied by a single episode of vomiting’. The patient did not have chest pain when assessed, and was also noted to be moving around the house.
2.8 The paramedic carried out a 12-lead ECG. The ECG’s auto-diagnostic function detected an abnormal cardiac finding based on the data profile of a ‘40 plus year old male’. The ambulance crew documented no abnormalities and the patient was discharged, with advice to re-contact emergency services if her symptoms worsened.
2.9 Later the same day another emergency call was received. The same ambulance crew went to the patient, supported by another two crews. On arrival, the paramedic began advanced life support and the patient was taken to the local emergency department, but died later the same afternoon. The patient’s cause of death was recorded by HM Coroner as a myocardial infarction (heart attack (MI)).
2.10 The trust’s incident report found that the ambulance crew acknowledged the ECG findings during the initial examination, but did not consider them a true representation of the patient’s symptoms. The patient did not have active chest or back pain or shortness of breath. The crew did not consider the monitor/defibrillator’s’ auto-diagnostic function to have been accurate. This was because they had previous experiences involving inaccurate readings from auto-interpretation software due to interference, such as patient movement.
2.11 The trust’s incident report referred to guidance by the Joint Royal Colleges Ambulance Liaison Committee (2019), which states:
‘A normal 12-lead ECG alone must not be used to exclude ACS [acute coronary syndrome]. The 12-lead ECG should be repeated, automated ECG interpretation can be a useful tool and the acknowledgement that whilst women do generally suffer from chest pain when experiencing an MI, there are occasions in this demographic where chest pain will not be evident.’
Patient 3
2.12 An ambulance crew was called out to a man, aged 33, who was experiencing chest pain and vomiting. On arrival the crew, comprising a newly qualified paramedic and EMT, noted that the patient appeared anxious, clammy, had quick speech and no difficulty in breathing.
2.13 The patient explained to the crew that he took regular medication for anxiety and had previously had panic attacks. However, he said he had run out of his medication and had not taken it for 2 days. He stated that he had previously had episodes similar to the one he was experiencing that day, as a result of not taking his anxiety medication.
2.14 An ECG was carried out (on a machine that did not have auto-interpretation software activated) which was interpreted by the ambulance crew as sinus tachycardia (a normal heart rhythm where the heart beats faster than usual).
2.15 The ambulance crew’s clinical impression was that the presentation was non-cardiac chest pain due to possible anxiety. Other factors highlighted in the trust’s investigation report were that the crew did not think the patient’s signs and symptoms were heart related, due to the patient’s young age and the other social factors and stressors he had talked about.
2.16 The patient was taken to the local emergency department and his care was handed over to hospital staff. The patients condition was monitored and the ECG was reviewed, at which point the hospital consultant recognised that the patient was having a STEMI. The patient went into cardiac arrest before transfer to a specialist primary percutaneous coronary intervention (PPCI) centre could be arranged. Resuscitation was attempted but was unsuccessful and the patient died at the hospital.
2.17 The trust’s incident report noted that if the STEMI had been recognised the crew could have discussed the patient’s case with the PPCI centre team. If the PPCI centre was not able to accept him, the patient would have been taken to the nearest emergency department, under emergency road conditions, with a pre-alert to ensure rapid assessment on arrival.
2.18 The trust’s incident report noted the possibility of incorporating recognition software onto the trust’s ECG devices to reduce the impact of ‘human error’ in ECG interpretation.
3. Analysis and findings
This section sets out the investigation’s analysis and findings in relation to how ambulance crews identify ST elevation myocardial infarction (STEMI). It considers the interpretation of 12-lead electrocardiograms (ECGs), and the monitor/defibrillator equipment and clinical support available to ambulance crews to help them interpret ECGs.
The first HSSIB report (Health Services Safety Investigations Body, 2025) which explored the education and training of paramedics in relation to 12-lead ECG, acknowledged the complexity of heart rhythms and clinical presentations of patients. This makes the process of undertaking an ECG more complex too. The report also discussed the importance of assessing a patient’s clinical signs, symptoms and medical history alongside interpreting the ECG trace, to provide a holistic assessment that would assist in diagnosing a STEMI.
The investigation heard that it was easy to interpret obvious or “barn door” STEMIs from a 12-lead ECG. However, it was more challenging to identify a STEMI where patients had less obvious signs and symptoms. This investigation looked at the equipment and support systems in place that were used by, and assisted, ambulance crews in diagnosing STEMIs. The analysis and findings are presented under the following headings:
- Monitor/defibrillator equipment and auto-interpretation
- Clinical advice and support in ambulance services
- Clinical advice and support from primary percutaneous coronary intervention (PPCI) centres.
3.1 Monitor/defibrillator equipment and auto-interpretation
Equipment design
Usability of ECG function in the environment and context they are used
3.1.1 The investigation found there were factors that impacted on the usability of equipment associated with the environment and context in which ambulance crews have to carry out ECGs. Paramedics told the investigation that they did not see and treat patients “on an examination table” or in “perfect position”. Instead, the reality of attending chest pain calls meant treating patients in a variety of settings including in their homes, sometimes in cluttered environments, and in more extreme environments such as “on the beach at 00:30 hours ... freezing”.
3.1.2 Every environment posed different challenges for the equipment, as this may affect the condition of the patient’s skin (being sweaty or cold can prevent the electrodes from sticking and gaining an accurate signal) or the available light for things like reading and interpreting the ECG printout (trace). Crews often reported having interference or ‘artefacts’ on the ECG trace, which affected the quality of the ECG trace and ease of interpreting a STEMI.
3.1.3 An artefact is a mark on an ECG trace that does not originate from a cardiac source. Artefacts were reported to come from other nearby electrical devices and/or from patient movement. One crew member told the investigation that they try to tell the patient to stay still, but still get movement which causes a lot of artefact on the ECG trace. As a result, they feel the ECG trace can be unreliable. Any perceived unreliability of the ECG trace can then negatively impact on ambulance crews’ decision making in diagnosing a STEMI.
3.1.4 A manufacturer told the investigation it had been looking into incidents where its monitor/defibrillator had given a false positive report (where the automated ECG interpretation incorrectly reported a cardiac abnormality). It found that artefacts were the main reason for the incorrect readings and was looking into this.
Readability of ECG printouts
3.1.5 ECG traces cannot be read accurately on the screen of monitor/defibrillator devices due to the smaller size, layout and information presented. Instead, the ECG trace must be printed out, either from an inbuilt printer or by pairing with a compatible portable printer. The investigation heard that some newer monitor/defibrillator devices supported ECG traces being read on compatible computer tablets where they could be enlarged; however, the investigation did not find these devices were widely in use.
3.1.6 The investigation found there was variability in the ECG printouts that the monitor/defibrillator devices produced, with some described as being easier to interpret than others. The ECG trace from each device was printed on different sized strips of paper; those on larger strips were more readable than those on smaller strips. There were also differences in the thickness of the lines of the trace, which made it more difficult for the ambulance crews to accurately measure and therefore interpret the ECG.
3.1.7 Some of the printouts showed additional information, such as measurements for the amplitude (strength of the electrical signals) of the ST segment, and the amplitude in the different leads, which helped the ambulance crews to interpret the ECG. Other printouts did not display this information and so crews would have to analyse and measure the graph themselves, by either counting squares or using a ruler, to obtain the same information.
3.1.8 This variability was a particular challenge when professionals transferred between ambulance services, or where different equipment was being used within the same service, and professionals may not be familiar with the specific ways in which information was displayed on different equipment. There is a need for further consideration of the impact the design and layout of the printout has on ECG readability and interpretation, as this can affect ambulance crews’ ability to identify and diagnose a STEMI.
HSSIB makes the following safety observation
Safety observation O/2025/075:
Regulatory bodies can improve patient safety by supporting standardisation across manufacturers in how information from ECG traces is displayed.
Auto-interpretation software
3.1.9 A review of nine ambulance trust investigations into a missed STEMI showed that there was only one incident where the auto-interpretation had stated ‘STEMI’. In the other incidents, the auto-interpretation had stated there was an abnormality of some description. As such, the auto-interpretation had not always provided a high level of clarity to support crews in their overall decision making and diagnosis.
3.1.10 There were some differences in ambulance crews’ perspectives about the accuracy of ECG auto-interpretation and how much reliance they placed on it. A few ambulance crew members stated that auto-interpretation was accurate and had improved over the years. However, the investigation found that in the main, ambulance crews did not trust auto-interpretation, including for diagnosis of STEMI. This potentially limited the reliability of the support available to ambulance crews while on scene with a patient, to help them correctly diagnose a STEMI and take the patient to the right place of care.
3.1.11 The investigation heard of instances where the auto-interpretation had been misleading, indicating that a patient was having a STEMI when they were not. In other cases, the auto-interpretation had reported the ECG as normal when it was not.
3.1.12 Manufacturers of monitor/defibrillators told the investigation that the auto-interpretation function was not there to replace clinical expertise. Manufacturers stated in their device guidance that the ECG should be reviewed by ‘qualified medical personnel’, a ‘physician’ or ‘doctor’. One manufacturer’s guidance stated that auto-interpretation is ‘no substitute for the qualified judgement of a properly trained, supervised clinician’.
3.1.13 The investigation found there were a number of factors that influenced the accuracy of, and ambulance crews’ trust of, auto-interpretation in diagnosing a STEMI. These factors are described in the following sections.
Accuracy of the auto-interpretation algorithm
3.1.14 Monitor/defibrillator manufacturers use different algorithms to analyse and interpret the ECG in their auto-interpretation software. The investigation explored some of the algorithms used and found there was variation in the amount of evidence and research the algorithm developers had to support the accuracy of the algorithm.
3.1.15 Algorithm accuracy data provided on manufacturers’ websites discussed algorithms’ sensitivity (the ability to correctly identify patients with a STEMI) and specificity (the ability to correctly identify those who do not have a STEMI). Most algorithms the investigation explored had a high level of specificity (between 94% and 100%) and so were highly accurate in correctly identifying patients who were not experiencing a MI. Accuracy levels for sensitivity were more variable, with data showing between 77% and 92.8% sensitivity for identifying a STEMI. This means that algorithms have a high rate of correctly identifying that a patient is not having a MI, but they were not as good at identifying a STEMI.
3.1.16 Accuracy data from one algorithm showed that for borderline STEMIs, sensitivity lowered to around 37% to 47%, meaning that the algorithm was not as good at identifying borderline STEMIs. Borderline STEMI was described as ECGs that show abnormal ST deviations, but do not meet the STEMI thresholds stated in American College of Cardiology/American Heart Association guidelines (American Heart Association, 2025), which align with the criteria used in England (see 3.3.1).
Auto-interpretation and protected characteristics
3.1.17 There can be differences in ECG traces depending on a patient’s age, sex and ethnicity (Macfarlane, 2018; Simonson, 1972). The investigation found potential misunderstanding within ambulance crews of how the auto-interpretation worked and what details were important for the auto-interpretation. For example, one paramedic stated that they did not think the patient’s age and sex influenced the auto-interpretation.
3.1.18 The investigation was told that the age and sex of a patient were not always entered into the ECG device. This was the case in patient story 2 (see 2.7 to 2.11). The investigation found that some monitor/defibrillator devices prompted crews to enter information on age and sex, while some devices did not. Where devices did provide such prompts, crews stated that they were easy to override and skip with the press of a button.
3.1.19 The investigation learned that if the age and sex of a patient is not entered into the ECG device, the auto-interpretation defaults to the setting of a male aged 45 or 50 years old. The auto-interpretation may then provide an incorrect analysis for that patient. HSSIB’s first ECG report (Health Services Safety Investigations Body, 2025) also highlighted the importance of considering protected characteristics when educating and training paramedics in ECG practice.
HSSIB makes the following safety observation
Safety observation O/2025/076:
Manufacturers can improve patient safety by identifying the potential design barriers and enablers for ambulance crews entering information about a patient’s age or sex into a monitor/defibrillator. This could inform future device design to increase the likelihood that this information is entered when carrying out a 12-lead ECG using auto-interpretation.
3.1.20 The investigation found that the algorithms it reviewed accounted for the sex and age of the patient, but only one was reported to have the ability for a patient’s ethnic background to be considered in the auto-interpretation software. However, the ambulance services the investigation engaged with had not included this feature during procurement.
3.1.21 One manufacturer discussed how it had considered including ethnicity in its latest device, but decided not to include it in the device’s auto-interpretation. This was because the data on ethnicity was collected in specific geographical locations, which they believed did not give a representative picture of how ethnicity affects ECG readings globally. Based on this the manufacturer felt it may not be appropriate to base the algorithm on the population data used. Comments the investigation received on consultation suggested that organisations such as the European Society of Cardiology or the American College of Cardiology/American Heart Association may be able to support in providing additional data to support how ethnicity may be reflected in algorithms.
HSSIB makes the following safety observation
Safety observation O/2025/077:
Algorithm developers can improve patient safety by collecting data from different ethnic groups across different geographical locations to help increase the global representation and accuracy of auto-interpretation algorithms for STEMI.
Auto-interpretation and electrode placement
3.1.22 During interviews with ambulance crews and observation of their practice, it was noted that electrode placement could be inconsistent. Research has also identified a high level of variation in the placement of chest electrodes, which could alter the shape of the ECG waves (Gregory et al, 2021) and affect the ability of ambulance crews to diagnose a STEMI correctly.
3.1.23 The algorithms were developed on the basis of data being collected from electrodes placed on the patient’s chest and their wrists and ankles. The investigation was told about, and observed, electrodes being placed on the torso, which was the correct technique to use when only using the ECG for monitoring. However, for 12-lead ECGs being used for diagnosis, placing the limb leads onto a patient’s torso instead of their wrists and ankles altered the distances between the electrodes and the heart, and thus the waveform, which could again skew the readings and auto-interpretation. This meant there was a potential risk of reduced accuracy in the algorithm, affecting ambulance crews’ ability to diagnose a STEMI.
3.1.24 This also raised an issue about the accuracy of 12-lead ECGs, STEMI diagnosis and auto-interpretation accuracy for patients who do not have all their limbs, such as amputees or may experience tremor, such as those with Parkinson’s. Other considerations about accurate lead placement for 12-lead ECGs were identified in HSSIBs first report (Health Services Safety Investigations Body, 2025).
Algorithm updates
3.1.25 There was variation in how much the algorithms were being updated. One manufacturer stated that the algorithm its device used was established approximately 40 years ago and it was not aware of any updates. Another manufacturer described how it was working with the algorithm developer to make improvements to the algorithm. That manufacturer was collecting data to understand when the algorithm was returning false positives or false negatives so that it could address these issues. The investigation was told the manufacturer had made changes to the algorithm over the years and these were being incorporated into the software of its latest device, which was due to come to market.
3.1.26 However, algorithm updates were not made to the manufacturer’s older device which was already being used by ambulance services in England. This was because of the regulatory requirements and approvals that would be required to do so.
Clarity of auto-interpretation output
3.1.27 The investigation found that auto-interpretation software can produce interpretative statements (the results of the algorithmic analysis of a patient's ECG reading) in different ways. ECGs clearly meeting the criteria for STEMI would state this on the ECG printout. The investigation found that the way in which interpretative statements alerted the user varied. One presented in bold text, another in capitals, and some had an audio alert and a flashing light to alert the user of a STEMI. Other interpretive statements were provided that were indicative of the stage or type of myocardial infarction, which in some cases could signify the early or late stages of a STEMI or borderline STEMI.
3.1.28 Each device used a large amount of terminology and clinical language to describe the abnormalities it detected. For example, one manufacturer’s guide listed 12 pages of statements that can come from the device. This meant a large number of statements for ambulance crews to understand. In addition, none of the devices had been developed in the UK or specifically for the UK market. The investigation was told that the terminology used on the device did not always align with UK paramedic terminology.
3.1.29 The investigation learned from one manufacturer that it was doing work to improve the language used in auto-interpretative statements, particularly in relation to borderline STEMIs. This was to try and further support ambulance crews in 12-lead ECG interpretation and make it clearer that the patient may be experiencing a borderline STEMI.
Other considerations
3.1.30 While auto-interpretation can help to improve the chances of diagnosing a STEMI, its use can also have downsides if it is not fully understood and used appropriately.
3.1.31 As noted in HSSIB’s first ECG report (Health Services Safety Investigations Body, 2025), most higher education institutions do not teach their students how to use or manage the auto-interpretation functions. There was evidence that ambulance crews did receive training on the monitor/defibrillator device their ambulance services used.
3.1.32 However, the investigation did not have evidence as to the depth to which ambulance crews are trained in the use of auto-interpretation. The investigation found that some ambulance crews were aware of some of the complexities of using the auto-interpretation, while others were not. In many instances, ambulance crews described using auto-interpretation as a ‘back-up’ to check their own clinical decision making rather than using it to help inform their clinical decision making. The investigation also heard from some ambulance crews that they had been taught not to read auto-interpretation due to its inaccuracy.
3.1.33 Having to manage both aspects of the task – the manual interpretation and the auto-interpretation and what that means for the overall diagnosis – can add to demands placed on ambulance crews by increasing the number of tasks they need to carry out. The investigation did not assess the workload or task demands associated with ambulance crews having to consider both manual and auto-interpretation as part of their clinical decision making. However, it was the opinion of some ambulance crew members and organisations that auto-interpretation should be switched off.
Initial monitor/defibrillator equipment design and procurement
3.1.34 The investigation considered how ambulance crews, both for clinical diagnosis but also usability, are considered in the design of monitor/defibrillators. This section also considers how the procurement process assesses the design, usability and auto-interpretation software when selecting products to put on the NHS Supply Chain framework and/or procure into ambulances services.
3.1.35 Overall, the investigation found limited evidence that the factors discussed in the previous two sections of this report were considered or could be sufficiently tested as part of the NHS Supply Chain or ambulance services’ procurement process. These factors included:
- the usability of the monitor/defibrillator in the environment used
- the readability of the printout
- the auto-interpretation.
Consideration of the user in product design and evaluation
3.1.36 All the manufacturers the investigation engaged with discussed how they considered the users of their monitor/defibrillator. New devices tended to evolve from previous versions, but with improvements made based on the clinical needs of ambulance services and understanding what ambulance services do. It was reported that the work of ambulance services has changed and so the device has changed with it. For example, over time customers required more monitoring capability. The investigation was told that most of the time, the device was now used for monitoring and so more emphasis had been placed on the design of this function.
3.1.37 When considering user requirements, manufacturers described using focus groups of paramedics from countries that have the biggest market share of their product. The UK was included in each of the manufacturer’s lists that they stated had an input, through feedback and focus groups, into the design process of the equipment. Paramedics were asked to feed back about previous products, for example what they liked or disliked about the device. The manufacturers were all keen to find out what future functionality was wanted and which functions needed to be improved.
3.1.38 Some manufacturers noted that any changes to the design of their device, which they said included updates to the algorithm software, would require it to be approved for use by meeting the Medical Device Regulations (MDR) and other international regulatory approvals again. Therefore, the cost/benefit of making improvements to current products was not always feasible. This also meant that updates were not always made available to ambulance services with older monitor/defibrillators, even if a software update was a possibility.
3.1.39 However, one manufacturer described that it was able to make changes to the device’s software and offer updates to current users of its device without having to go through the full approval process.
3.1.40 The investigation noted that globally there are multiple regulatory requirements and approvals device manufacturers have to meet to bring a product to market in a particular country or region. This adds complications to updating equipment that has been sold meeting different regional regulations.
3.1.41 The manufacturers reviewed incidents that had been raised directly to them or through the Medicines and Healthcare products Regulatory Agency’s 'Yellow Card Scheme' (MHRA n.d.), (a reporting system for medicines, vaccines, medical devices, blood products and e-cigarettes), to learn of problems and make changes to their equipment. They also reviewed incidents raised via reviews of issues and complaints submitted by paramedics about faults or functionality.
3.1.42 However, the investigation was told that manufacturers do not receive many incident investigation reports. This limits their knowledge and understanding of how the monitor/defibrillator may be used in practice and how factors associated with the design or auto-interpretation software can influence patient safety and diagnosis of STEMI.
3.1.43 After speaking to ambulance crews, the Medicines and Healthcare products Regulatory Agency and manufacturers, it is likely that the reporting systems are not being used to report incidents other than those that lead directly to harm. This is reducing the opportunity for learning about errors and potential design issues (such as age/sex inputting difficulties) with the monitor/defibrillators.
HSSIB makes the following safety observation
Safety observation O/2025/078:
Ambulance services can improve patient safety by informing regulators and manufacturers of instances where the use of monitor/defibrillators has impacted on patient safety.
Procurement by NHS Supply Chain
3.1.44 NHS Supply Chain manages the sourcing, delivery and supply of healthcare products. It lists products on its framework that are available for NHS organisations to procure, including monitor/defibrillators used by ambulance services. It should be noted that ambulance services are not required to source medical equipment from NHS Supply Chain and other routes are available; however, the investigation found that most ambulances services (90%) use NHS Supply Chain.
3.1.45 The investigation found that NHS Supply Chain lists the monitor/defibrillator that paramedics use to conduct 12-lead ECGs under its ‘External Defibrillation Devices and related Services and Accessories’ framework (NHS Supply Chain, 2023). It also has a ‘Cardiac Diagnostics Equipment, Technologies and Related Equipment and Services’ framework. However, this framework did not list the monitor/defibrillators that ambulance services are using to identify a STEMI as the device was considered to be primarily a defibrillator by NHS Supply Chain.
3.1.46 The investigation reviewed the NHS Supply Chain’s statement of requirements for the category of ‘Defibrillators’ which guides ambulance services in stating their requirements for a defibrillator. While the statement of requirements considers aspects such as functionality, displays, data management, accessories and safety, these did not appear to focus on the monitoring (aside from 3-lead ECG monitoring) or 12-lead diagnostic ECG functions of the device, such as the ease of use of these functions, how they displayed and alerted key information and aspects such as the reliability of the auto-interpretation software.
3.1.47 NHS Supply Chain told the investigation it was working through improving its human factors assessment of devices and how it could share details in a way that was helpful to customers. NHS Supply Chain reported that it can struggle to get rich information or data on device complaints or user issues which would be useful to help in the assessment of devices. The need for better triangulation of such information was highlighted.
Procurement of monitor/defibrillator devices into ambulance services
3.1.48 The investigation spoke to ambulance trusts about their procurement process, including one trust which was procuring a new suite of monitor/defibrillators at the time. The trust described processes that involved paramedics testing the equipment in simulation scenarios, but it was unable to test it in real scenarios and with teams who may be tired and under stress at the time.
3.1.49 Each trust developed a list of system requirements; an example can be seen in figure 6. They then also developed a weighting system for each of the system requirements.
Figure 6 Ambulance trust monitor/defibrillator assessment scoring sheet
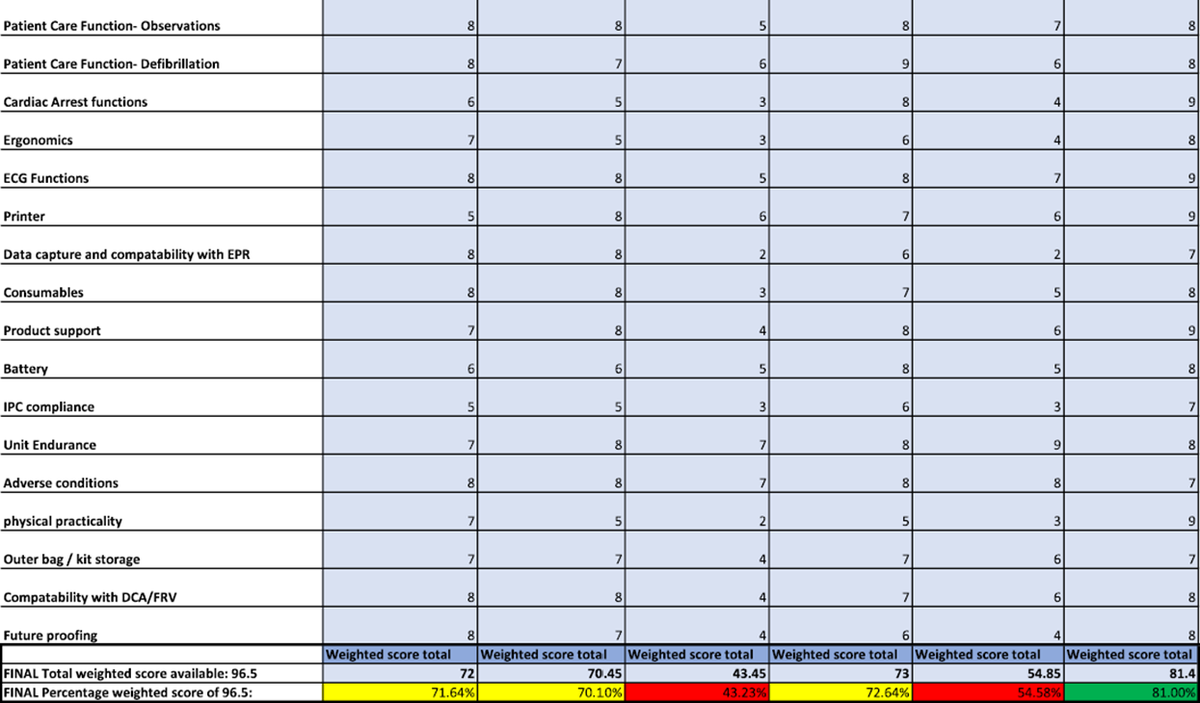
3.1.50 The investigation reviewed the scoring sheet shown in figure 6 and found that it was not clear from the table what weighting had been applied to each system requirement. There are 17 categories in the table and there is no explanation as to whether each category carries the same weighting, or if some are considered more important and therefore have a higher weighting applied to them in the scoring. NHS Supply Chain told the investigation that the scoring and weighting was down to each ambulance service and there was variability in how this was carried out.
3.1.51 The example in figure 6 was also compiled before a new mandatory government guideline in the ‘Procurement policy note (PPN) 002’ was implemented, which states ‘PPN 002 mandates a minimum weighting for social value of 10% of the total scores available (or equivalent)’ (GOV.UK, 2025). The social value includes three aspects:
- economic (such as employment or apprenticeship/training opportunities)
- social (activities that promote cohesive communities)
- environmental (such as efforts in reducing carbon emissions).
3.1.52 With 90% of the scoring weight remaining, it is important to ensure that the weighting is placed correctly so the equipment meets trusts’ specifications and therefore the needs of the ambulance crews who use it. The investigation noted that physical attributes, such as physical practicality (weight and size) and equipment storage, were all scored individually; at least six of the categories could be classed as physical attributes.
3.1.53 However, the clinical aspects of ECG functions were covered in one category, with no consideration to splitting this into more categories, such as ECG trace readability and auto-diagnostic algorithm performance. The same could be said for the ‘cardiac arrest functions’ category. These are the key functions used by ambulance crews on every shift, but have less weighting and influence in the scoring system than the physical attributes.
3.1.54 One ambulance trust told the investigation that it does not replace its devices all at once; it does so gradually over time with like-for-like replacements. To that end, it does not go through a full procurement process. This approach negated the trust’s ability to assess other devices for advances in technology, such as improvements to the auto-diagnostic algorithms, ECG trace printout quality, and new clinical functions.
3.1.55 When considering the evolving nature of monitor/defibrillator devices and them being used more for their monitoring function, than the defibrillation function, the procurement processes seen by the investigation had not kept up with these changes. While the investigation acknowledged that each element of the scoring system was important, from the perspective of a paramedic trying to diagnose health problems being shown on an ECG trace, it was not clear that this and the other clinical functions were being prioritised during the procurement process.
HSSIB makes the following safety recommendation
Safety recommendation R/2025/071:
HSSIB recommends that NHS Supply Chain reviews and amends the procurement framework for monitors/defibrillators to help ambulance services ensure they are fully considering the defibrillation/monitoring and cardiac diagnostic functions of the device when making purchasing decisions, to better reflect how these devices are used in practice.
3.2 Clinical advice and support in ambulance trusts
Evolution of the ambulance trust clinical support hub
3.2.1 Ambulance trusts across the country have set up advice or support functions to assist ambulance crews, when they are on scene with patients. The nature of the set-up varied between trusts and was aimed at providing advice and guidance to a number of different levels of crew experience, depending on the trust that the investigation spoke to.
3.2.2 Some trusts told the investigation that the purpose of support hubs had evolved over time. One trust said the support hub was initially intended to support newly qualified paramedics (NQPs) with some decisions they had to make during their initial period of training, when they had limited experience.
3.2.3 The NQPs found this service particularly useful while they were gaining experience in reading ECGs. They stated that while they could identify heart rhythms and obvious STEMI readings, they struggled with less obvious STEMI readings. In their view, having a more experienced paramedic to go to for advice, confirmation or a second opinion was invaluable. An NQP that the investigation spoke with said that “in the absence of other expert advice, the paramedics relied on their colleagues [in the support hubs]”.
3.2.4 Ambulance crews stated that while contacting the support hub helped, staff at the hub did not have access to the patient's recorded medical history or have sight of the patient, which meant they did not have a holistic view of the patient. While a second opinion was often beneficial it was imperative that, for better decision making about treatment and diagnosis of the patient, the paramedic on scene led the conversation and took the holistic view into account.
3.2.5 Over time, the role of the ambulance service support hubs had evolved. Increasingly they were being used by experienced paramedics to seek advice or a second opinion on a diagnosis, particularly to help with ECG interpretation. Staff at the hub did not have the same pressures and environment complications experienced by crews at the scene with patients. However, the hub visited by the investigation was noisy and not a peaceful environment to quietly review an ECG that had been sent in (by phone, iPad or computer). Therefore, there were advantages and disadvantages for crews and hub staff when reviewing and confirming a diagnosis from ECG traces.
ECG interpretation and advice
3.2.6 In HSSIB’s first ECG report, which looked at paramedic training in respect of reading and understanding ECG traces (Health Services Safety Investigations Body, 2025), the phases of training were laid out, from paramedics’ university course to their induction training and then on-the-job training after joining an ambulance trust. Ambulance crews at all these levels stated that they valued the shared decision making that the hubs offered for more complex patients and difficult diagnoses.
3.2.7 The set-up and staffing of support hubs varied across the country, with some staffed by paramedics of the same grade as the paramedics who were responding to emergencies and calling the hub for advice. At other hubs more senior clinicians were available to offer advice and support.
3.2.8 Hub staff may have been more experienced and have skills and training in other areas such as clinical decision making, but in terms of cardiology or reading and interpreting ECGs they had no further qualifications than the crews treating the patients.
3.2.9 The investigation was also given an example where a paramedic had been “working in the clinical advice line for 10 years, not [physically] seen a patient since… ECGs aren’t his thing … he’s been sent an ECG to [review and he’s said] well, I don’t know what to do with it”. This emphasises that any advice line must have the correct person, with sufficient knowledge and experience, at the end of the line to be able to review ECG traces and correctly diagnose patients.
3.3 Clinical advice and support from primary percutaneous coronary intervention centres
Acceptance criteria interpretation variation
3.3.1 NHS primary percutaneous coronary intervention (PPCI) centres receive and treat patients with a confirmed STEMI. There are criteria for confirming a patient is experiencing a STEMI based on the measurements and findings from an ECG trace (NHS England, 2013).
3.3.2 The investigation was told that the acceptance criteria worked well when it was clear on the trace that the measurements met the criteria for a STEMI. However, when the STEMI was evolving but had not yet reached the threshold, there was variability between PPCI centres as to whether they would accept the patient or not. Concerns were raised during stakeholder discussions that some patients who were experiencing a STEMI were not always being taken to the right place of care in time.
3.3.3 The investigation analysed nine serious incidents reports and found that in five incidents, the patient had been taken to an emergency department instead of a PPCI; this contributed to two of these patients dying. In four incidents, the patient had been discharged at their home; two of those patients subsequently died at home. The other two patients who had remained at home were later transferred to a PPCI; one died on the way to the PPCI.
3.3.4 These factors were particularly relevant in cases of borderline STEMIs where the most suitable place of care may not be clear based on the patient’s clinical signs and symptoms and interpretation of the ECG.
3.3.5 Ambulance crews told the investigation that the acceptance criteria and approach could vary across different PPCI centres. Some ambulance services included a number of PPCI centres within their geographical area, whereas some that were situated at the border with other ambulance service areas may find it necessary to take patients to PPCI centres outside of their region. Ambulance crews told the investigation that the acceptance criteria and approach they found at different PPCI centres could impact on their decision making about patients with a STEMI and where to take them.
3.3.6 Ambulance crews told the investigation that sometimes they would take a patient to a PPCI centre even if their ECG trace did not meet the criteria at the time, as from clinical experience they could recognise when it was likely that the ST elevation would meet the criteria by the time they arrived at the hospital. Making this decision without consultation with or agreement from the PPCI centre, regardless of whether it was the correct decision, did not allow the PPCI centre staff to prepare properly for a patient’s arrival.
3.3.7 The investigation spoke to consultant cardiologists (heart specialists) within PPCI centres who also gave differing views on when they would advise ambulance crews to bring a patient with a suspected STEMI to a PPCI centre. Some cardiologists said they would accept a patient who did not quite meet the ST elevation criteria in the knowledge that they were likely to do so once they arrived at hospital. Other cardiologists applied a strict boundary and would only accept patients if the ECG taken when the ambulance crew was at the scene with a patient already met the elevation criteria. One of the reasons for this was capacity and not being able to accept any cases that might be ‘borderline’ (where the criteria had not quite been met).
3.3.8 Ambulance crews and cardiologists also told the investigation that women and people with diabetes could show different signs and symptoms when suffering from a STEMI. Sometimes they would have no chest pain, which would mean they did not meet the criteria for admission to a PPCI centre. Again, there was variation among PPCI centre cardiologists as to whether sex or a diagnosis of diabetes would be taken into account when assessing if a patient met the criteria.
3.3.9 NHS England was, at the time of the investigation, in the process of producing updated guidance to try and remove variation between acceptance criteria and the interpretation of that criteria by PPCI centres, therefore reducing the confusion for ambulance crews. As the guidance was new it was too early for the investigation to assess whether it had achieved or would achieve its aim. However, this new guidance would not solve the issue of how PPCI centres, and their consultants, review and consider evolving STEMIs that have not yet reached the accepted written standards for acceptance.
Two-way communication
3.3.10 When ambulance crews were unsure about the interpretation of an ECG trace, or were unsure if a patient met a PPCI centre’s acceptance criteria, they would often seek advice from the PPCI centre about whether the patient was suitable for transfer to them for treatment (two-way communication). The investigation was told there was variation between PPCI centres, and between teams within PPCI centres, in their willingness to review ECG traces or give advice to ambulance crews.
3.3.11 The investigation was also told by a cardiology consultant that the PPCI centres were “not commissioned to provide an advice line for ambulance crews” and therefore the capacity to provide this service effectively was often limited.
3.3.12 Some ambulance crews were told the PPCI centre is “not an advice line” and that they were “not there to interpret their ECGs” for them. A newly qualified paramedic confirmed this when they told the investigation that they did not consider calling the PPCI centre for advice during an incident, as “that’s not what they’re there for”. They also stated that they had recently been briefed by their ambulance service not to call the PPCI centre for advice.
3.3.13 Internationally there are alternative models of providing care and resourcing ambulance services, including the use of different clinicians or increased access to speciality knowledge. There may be elements of these models that may be considered to find improvements for services in England.
3.3.14 The investigation found that in Germany, federal law allows for telemedicine consultation in support of paramedic crews because “they cannot … get enough physicians to go out with every response”. This means an ambulance crew can conduct a diagnostic test, which is then reviewed by a ‘telemedic’ (consultant) via video. This removes the pressure from crews and ensures that a diagnosis and decision about where to transport the patient is made by a cardiology consultant.
3.3.15 This approach had two benefits to the wider healthcare system:
- The ambulance crews were assisted by a cardiology consultant in making an accurate diagnosis.
- The PPCI centre/hospital where the patient was being taken was confident that the patient had been diagnosed correctly and therefore if a PPCI team had been activated, it had been done so correctly.
3.3.16 The investigation heard varying evidence about two-way communication systems. One consultant cardiologist stated that while the format might vary, two-way communication was now operational between all ambulance services and PPCI centres.
3.3.17 In a survey of PPCI centres conducted by NHS England (2023) 86% of PPCI centres (55 of 64) responded that they had direct communications in place with ambulance services, although the survey did not ask or ascertain whether the communication routes were effective. Of those centres, 53 responded that they had a dedicated phone line for ambulance crews to call, with 48 of those having an identified staff member (24 hours a day) to answer that phone line. The identified staff members were:
- coronary care unit nurse (59%)
- specialist cardiac nurse (14%)
- cardiology registrar or other registrar (8%)
- cardiology consultant (2%)
- other (17%).
3.3.18 The survey painted a picture of a network of PPCI centres and ambulance services with most in regular communication. However, the investigation heard that this was not the case and was not the experience of many ambulance crews from different regions of the country. During discussions with ambulance crews as part of the investigation, two-way communication was not consistently reported. The investigation was also told that while some PPCI centres did take calls, they were not always taken by someone with greater ECG interpretation skills or experience than the crew. Some crews told the investigation that they would only be able to speak to a receptionist or a nurse who may not be a cardiology nurse.
3.3.19 The investigation heard that PPCI centres in England that had implemented effective two-way communication with ambulance crews had reduced the number of false activations of PPCI teams (where PPCI teams are activated for a patient who is not having a STEMI). A cardiology consultant stated that their organisation had implemented a 24/7 phone number for ambulance crews to speak to someone about patients with a suspected STEMI. The phone was staffed by a cardiology nurse during the day and by either a registrar or a consultant at night. The conversation on the phone was backed up by the ambulance crews transmitting the ECG trace to the PPCI centre for review. The percentage of false activations of PPCI teams at that hospital site had reduced from 33% to less than 5% since the introduction of the phone line.
3.3.20 While this led to a financial saving from not calling out PPCI teams, who may be at home, for example out of hours (true financial saving had not been calculated), there was a further, and important, benefit of PPCI teams being better rested for when they were needed. In addition, the consultant stated that this service had the added benefit of feedback and therefore learning for the ambulance crews. This learning was likely, in time, to reduce the number of calls and therefore negate any perceived burden created by the phone line.
3.3.21 In the service specification for PPCI centres there is no mention of a requirement to provide advice or assistance to ambulance crews when assessing patients for suitability for transfer to a PPCI centre. However, with some trusts having a false activation rate of approximately 50%, a change to the current system would be beneficial for both ambulance crews and the PPCI centres’ PPCI teams.
HSSIB makes the following safety recommendation
Safety recommendation R/2025/072:
HSSIB recommends that NHS England/Department of Health and Social Care reviews and amends the service specification for primary percutaneous coronary intervention (PPCI) centres, to include a requirement for a function enabling two-way communication with ambulance crews for shared decision making about patients with a suspected STEMI. This is to ensure that patients are taken to the correct place of care and PPCI teams are responding to confirmed STEMI cases.
4. References
American Heart Association (2025) ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction. Available at https://www.ahajournals.org/doi/10.1161/01.cir.0000134791.68010.fa (Accessed 6 August 2025).
Carayon, P., Schoofs Hundt, A., et al. (2006) Work system design for patient safety: the SEIPS model, Quality and Safety in Health Care 2006; 15(Suppl I): i50–i58. doi: 10.1136/qshc.2005.015842
Courts and Tribunals Judiciary (n.d.) Reports to prevent future deaths. Available at https://www.judiciary.uk/courts-and-tribunals/coroners-courts/reports-to-prevent-future-deaths/ (Accessed 16 December 2024).
GOV.UK (2025) Guide to using the social value model. Available at https://www.gov.uk/government/publications/ppn-002-taking-account-of-social-value-in-the-award-of-contracts/ppn-002-guide-to-using-the-social-value-model-html (Accessed 12 June 2025).
GOV.UK (2025) Regulating medical device in the UK. Available at https://www.gov.uk/guidance/regulating-medical-devices-in-the-uk (Accessed 28 May 2025).
Gregory, P., Kilner, T., et al. (2021) Accuracy of ECG chest electrode placements by paramedics: an observational study, British Paramedic Journal, 6(1), pp. 8–14. doi: 10.29045/14784726.2021.6.6.1.8
Health Services Safety Investigations Body (2025)12-lead electrocardiograms (ECGs) in ambulance services: paramedic education, training and competence. Available at https://www.hssib.org.uk/patient-safety-investigations/pre-hospital-interpretation-of-electrocardiograms-ecg-in-ambulance-services/investigation-report/#background (Accessed 3 June 2025).
Joint Royal Colleges Ambulance Liaison Committee (2019) JRCALC clinical guidelines.
Macfarlane, P.W. (2018) The influence of age and sex on the electrocardiogram, Advances in Experimental Medicine and Biology Journal, 1065, pp. 93-106. Available at https://pubmed.ncbi.nlm.nih.gov/30051379/ (Accessed 16 December 2024).
Medicines and Healthcare products Regulatory Agency (n.d.) About the Yellow Card scheme. Available at https://yellowcard.mhra.gov.uk/about-yellow-card (Accessed 5 June 2025).
National Institute for Health and Care Excellence (2020) Acute coronary syndromes. NICE guideline [NG185]. Available at https://www.nice.org.uk/guidance/ng185/chapter/Recommendations#stemi-early-management (Accessed 21 July 2025).
NHS England (2013) 2013/14 NHS standard contract for cardiology: primary percutaneous coronary intervention (PPCI) (adult). Available at https://www.england.nhs.uk/wp-content/uploads/2018/08/Cardiology-primary-percutaneous-cortonary-intervention-adult.pdf (Accessed 28 July 2025).
NHS England (2023) Survey of primary PCI centres – communications with ambulance services for suspected STEMI. (Unpublished)
NHS Supply Chain (2023) External defibrillation devices and related services and accessories. Available at https://www.supplychain.nhs.uk/product-information/contract-launch-brief/external-defibrillation-devices-related-equipment-and-associated-accessories/ (Accessed 28 July 2025).
Simonson, E. (1972) The effect of age on the electrocardiogram, The American Journal of Cardiology, 29(1), pp. 64–73. doi: 10.1016/0002-9149(72)90417-1
5. Appendix
Investigation approach
The investigation reviewed multiple sources of evidence to help identify risks that may be posed to patient safety in relation to paramedic recognition of ST elevation myocardial infarction (STEMI) via 12-lead electrocardiograms (ECGs). These included:
- national incident reporting systems
- academic literature
- national and international publications.
The investigation also engaged with a wide range of stakeholders (see below) to learn more about the issues surrounding ECG interpretation and identify areas on which an investigation could focus to help improve patient safety. The way 12-lead ECGs are undertaken and interpreted was identified as a growing area of concern, with systemic safety risks that can have a significant impact on the outcome for patients.
Multiple stakeholders highlighted specific challenges in interpreting ECGs for patients with chest pain. In particular, concerns were raised about diagnosis of STEMI, as the most serious form of heart attack, which poses the greatest risk to patients.
HSSIB searched the Strategic Executive Information System (StEIS), which is a national database for reporting serious safety incidents in healthcare. The incident data reviewed also suggested a significant impact particularly when it came to STEMI, with 30 of 52 incidents (58%) between January 2022 and January 2024 involving STEMI or suspected STEMI. Of these 52 incidents, 40 involved the death of the patient, thus demonstrating a significant outcome impact on patient safety.
Evidence gathering
The investigation visited 5 out of 10 ambulance services in England, based on the different type of ECG equipment being used, and engaged with a selection of specialist treatment centres providing primary percutaneous coronary intervention – PPCI.
Patient safety incident reports relating to incorrect ECG interpretation were requested from ambulance services and reviewed alongside incidents reported on StEIS to understand some of the common emerging safety themes. The investigation team also spoke to representatives from primary percutaneous coronary intervention (PPCI) centres.
Semi-structured interviews were conducted, guided by the Systems Engineering Initiative for Patient Safety (SEIPS) framework. The SEIPS framework was also used as a guide during site visits for evidence collection and in the thematic analysis of all the data gathered. SEIPS provides a human factors framework for understanding the work system (that is, the external environment, organisation, internal environment, tools and technology, tasks, and people), work processes (including physical, cognitive and social/behavioural aspects) and the relationship between these and the resulting outcomes in healthcare (Carayon et al, 2006).
Stakeholder engagement and consultation
The investigation engaged with many stakeholders and subject matter advisors to gather evidence during the course of the investigation. This also enabled checking for factual accuracy and overall sense-checking. The stakeholders contributed to the development of the safety recommendations based on the evidence gathered and are listed below.
| Reference and comparison site organisations | Staff | National organisations | Subject matter advisors |
|---|---|---|---|
| 5 ambulance services in England |
Newly qualified paramedics Paramedics Ambulance service managers Paramedic safety specialists 2 ambulance service procurement teams |
NHS England | Consultant paramedic |
| 3 PPCI centres | 3 cardiology consultants | Medicines and Healthcare products Regulatory Agency | Academic with interest in ECG auto interpretation algorithms |
| NHS Supply Chain | |||
| Monitor/defibrillator manufacturers and suppliers |